Capítulo 19 - Insuficiencia Venosa Crónica
La insuficiencia venosa crónica se define como elfuncionamiento anómalo del sistema venoso causado por insuficiencia valvular venosa, con o sin obstrucción deldrenaje venoso, y que puede afectar al sistema venoso superficial, al profundo o a ambos. Suponen un altísimo porcentaje de población adulta afectada, un alto coste económico para su tratamiento y una pérdida importante anual por bajas laborales.
19.1 Fisiopatología
Parece cada vez más claro que el desarrollo de una insuficiencia venosa crónica tiene un componente genético estimulado por factores ambientales. La fibrosis de la pared venosa y la pérdida de la competencia valvular hacen que se desarrolle una hipertensión venosa en los pacientes susceptibles. La transmisión de la hipertensión venosa a la microcirculación dérmica causa extravasación molecular y de glóbulos rojos que sirven como desencadenante de mecanismos inflamatorios locales. El siguiente paso es la activación de citoquinas y factores del crecimiento quefavorecen la migración de leucocitos hacia el intersticio. La secreción de TGF-B1 por los leucocitos y la unión posterior a fibroblastos produce fibrosis dérmica y remodelación tisular. A medida que avanza la enfermedad se produce una disminución de fibroblastos y una pérdida de capacidad para regenerar las lesiones cutáneas.
TABLAS
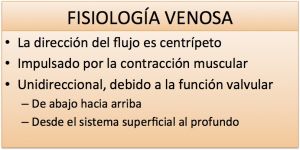
Tabla 1. Recuerdo fisiológico
19.2 Clasificación
Como la etiología, anatomía y fisiopatología de la insuficiencia venosa crónica son muy variables se ha diseñado un sistema de clasificación aceptado internacionalmente que nos permite establecer una evaluación inicial y nos sirve de comparación para la posterior evolución. El sistema de clasificación CEAP consta de 6 síntomas, 17 zonas anatómicas y categorías etiológicas y fisiopatológicos tripartitas (1994 a iniciativa del American Venous Forum). Sus siglas corresponden a C (clínica), E (etiología), A (anatomía) y P (fisiopatología). En la práctica médica diaria el sistema más utilizado es solo la clasificación clínica (C).
C0Asintomático sin anomalías visibles.
C1 Telangiectasias (venas de < 1 mm de diámetro).Venas reticulares (< 4 mm diámetro).
Fig. 1 Telangiectasias
Fig. 2 Variz reticular
C2Varices palpables de > 4mm de diámetro
Fig. 3 Varices
C3 Edema sin cambios cutáneos.
Fig. 4 Edema pierna izquierda
C4Cambios cutáneos sin úlcera. Incluidos los eccemas húmedos o secos.
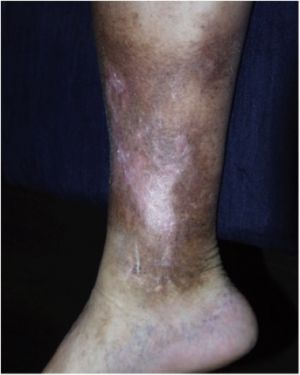
Fig. 5 Cambios tróficos
C5 Úlcera curada.
Fig. 6 Estigmas cutáneos de úlcera curada
C6 Úlcera activa.
Fig. 7 Úlcera venosa
Fig. 8 Gran úlcera maleolar
Las tres categorías etiológicas se excluyen mutuamente: primaria, secundaria y congénita.
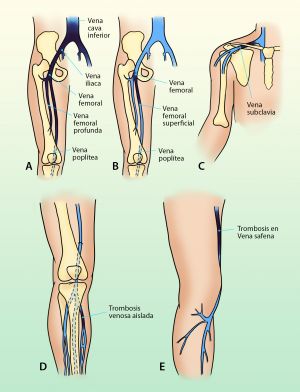
La clasificación anatómica divide las anomalías de los tres sistemas venosos de los miembros inferiores: superficial, profundo y perforantes.
La clasificación fisiopatológica establece 3 grupos: reflujo, obstrucción o ambos.
Existen otras enfermedades médicas que pueden presentar características similares a la insuficiencia venosa crónica y con las que debemos establecer el diagnóstico diferencial. Así cuando existe edema hay que descartar la existencia de insuficiencia cardiaca, renal o hepática, hipoproteinemia o anemia. La pigmentación y dermatoesclerosis puede existir también en el mixedema crónico, obesidad mórbida, insuficiencia cardiaca o ascitis. La úlcera crónica puede aparecer también el la obesidad mórbida, necrobiosis diabética, enfermedades reumáticas, discrasias sanguíneas y neuropatías periféricas. Raramente hoy día la TBC, sífilis o lepra pero puede aparecer en psoriasis. Finalmente hay que diferenciarlas de lesiones por picaduras de insectos, gota, tumores malignos, vasculitis, isquemia arterial,…etc.
En este tema vamos a hablar del tipo más frecuente de insuficiencia venosa crónica: las varices.
19.3 Varices
19.3.1 Definición
Son dilataciones de las venas superficiales que con frecuencia son tortuosas, dilatadas y se presentan principalmente en miembros inferiores (Organización Mundial de la Salud).
19.3.2 Epidemiología
Existen numerosos estudios epidemiológicos, generalmente centrados en un marco geográfico o laboral muy delimitado, que nos muestran una prevalencia que oscila entre el 15% y el 56% de la población general. Estas diferencias tan significativas se deben a lo que cada autor ha considerado como varices. Si incluimos en este término las arañas vasculares (telangiectasias), las varices reticulares y las grandes dilataciones varicosas la cifra se aproxima al porcentaje mayor, pero si por el contrario solo consideramos las grandes varices la prevalencia se acerca más al 15%.
Si en vez de tomar en cuenta su aspecto las agrupamos por el grado de severidad clínica nos encontraremos que el 44% de estas varices son irrelevantes para la salud y solo un 12% tienen verdadera repercusión clínica (dolor, edemas, lesiones de la piel, hemorragias, flebitis,…).
Extrapolando los datos a España debemos sospechar que entre 6 y 23 millones de personas padecen alguna forma de varices y al menos 5 millones precisarían tratamiento médico o quirúrgico. En el grupo de edad entre 30 y 70 años, que incluye a la mayoría de la población laboral, el 40% presenta alguna forma de varices, el 15% con relevancia clínica y el 1’5% llega a desarrollar úlceras venosas en las piernas.
19.3.3 Factores Asociados
Varios factores favorecen o aumentan el riesgo de desarrollar varices:
1.-La edad. Es el principal factor de riesgo y afecta por igual a hombres y mujeres. A los 70 años el 70% de la población presenta algunos de los tipos
de varices descritos, un 55% entre las personas con edades comprendidas entre los 55 y 64 años y menos del 10% en menores de 30 años.
2.- La herencia. Los portadores de varices tienen una historia familiar dos veces más frecuente que los no portadores. Estudios recientes del genoma humano han demostrado que las personas que padecen varices tienen sobreexpresión de los genes relacionados con el metabolismo del ácido araquidónico y de mediadores de la reacción inflamatoria (HPGD) así como infraexpresión de los genes relacionados con la producción de colágeno. Además se ha encontrado que múltiples genes de función aún desconocida son completamente distintos en pacientes que sufren insuficiencia venosa de aquellos que no la padecen.
3.- La obesidad. Juega un papel desfavorable en ambos sexos por igual.
4.- Embarazos múltiples. Entre grupos de mujeres de 37 años, uno sin haber sufrido embarazos y el otro con dos embarazos, hay cuatro veces más varices en el grupo de las embarazadas que en el otro.
5.- El género. Aunque la mujer consulta 9 veces mas que el hombre por varices, éstas, cuando son tronculares, son igual de frecuentes en ambos sexos, sin embargo las arañas vasculares son más frecuentes en la mujer.
6.- Anticonceptivos orales. Pueden favorecer el desarrollo de varices aunque no de forma muy significativa y, en cambio, parecen proteger frente a las flebitis y los embolismos pulmonares.
7.- Las hernias. No favorecen en si mismas la aparición de varices pero si existe una asociación frecuente entre ambas enfermedades.
8.- El tipo de trabajo. Especialmente en profesiones con ortostatismo prolongado (mucho tiempo de pie) como camareros, panaderos, azafatas, profesores,…
9.- Problemas ortopédicos. Al igual que con las hernias existe una asociación significativa con las varices, especialmente en mujeres.
10.- La clase social. Las varices son más frecuentes en las clases medias-bajas y obreros industriales.
11.-El estreñimiento. Es posiblemente una de las causas frecuentes en las sociedades ricas y adictas a la comida basura rápida.
19.3.4 Fisiopatología
El elemento clave de la aparición y desarrollo de las varices es el deterioro o insuficiencia de las válvulas que existen a lo largo de las venas. No importa si primero se produjo una dilatación de la vena o si fue el fallo valvular, lo cierto es que se producen unos fenómenos mecánicos patológicos como son: aumento de la presión de la sangre sobre distintos segmentos de la pared de la vena, salida de líquido al exterior de la vena (extravasación plasmática), alteración del intercambio entre los sistemas intra y extravascular, aumento de la permeabilidad capilar que producirá edema, aumento local CO2 y ácido láctico, liberación de histaminas, serotonina y prostaglandinas,… Esta cadena de acontecimientos es la responsable de la posterior sintomatología de las varices. Así el aumento de permeabilidad favorecerá la aparición de edema y la liberación de metabolitos dará lugar a dolor y procesos inflamatorios locales.
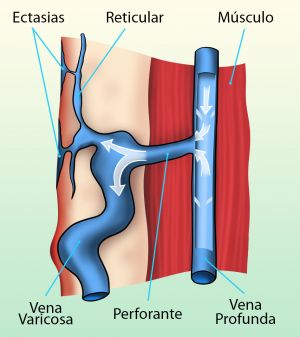
Fig. 9 Varices a expensas de venas perforantes
19.3.5 Clínica
Siguiendo el progresivo deterioro funcional que explicábamos en el párrafo anterior los síntomas cambiaran según avance la enfermedad. Habitualmente utilizamos una clasificación internacional en cuatro grados:
1º.- Se caracteriza por una rápida aparición del entramado venoso de las piernas, En general pueden verse varices en cara antero externa de muslos, detrás de las rodillas y en cara interna de piernas pero son asintomáticas.
2ª.- Las varices comienzan a producir molestias cuando se ha roto el equilibrio hidrostático, aparecen: pesadez y cansancio, sobre todo cuando se esta mucho tiempo de pie (ortostatismo) y al finalizar el día y mejora al pasear, con el ejercicio o cuando se elevan las extremidades; dolor , especialmente a lo largo de los trayectos varicosos, en pantorrillas y en los tobillos, su intensidad puede ser muy variable; calambres, sobre todo en pantorrillas y por la noche; prurito, o picores en tobillos y dorso del pie que pueden se puerta de entrada de infecciones a partir de lesiones de rascado; edema (hinchazón de piernas) que inicialmente son en tobillos y pie y pueden acabar afectando a la pierna, al principio ceden con el reposo pero con el tiempo tienden a cronificarse y no desaparecer.
3º.- Se caracterizan por la aparición de depósitos subcutáneos de hematíes que se caracterizan por manchas pardas en la piel. La degeneración de la piel y la grasa que existe bajo ella dan lugar a reacciones inflamatorias locales que acaban produciendo zonas endurecidas y dolorosas (fibrosis subcutánea).
4º.- En esta fase aparecen úlceras, generalmente en la proximidad de los tobillos, son muy dolorosas y tardan mucho en curar.
19.3.6 Exploración Física
Se debe realizar con las extremidades inferiores completamente desnudas y con el paciente en ortostatismo (de pie).
La simple inspección nos revelará la existencia de una red venosa superficial dilatada, su forma y su localización, también valoraremos el aspecto de la piel (manchas, eccemas, zonas induradas, úlceras, infecciones,…), la existencia de edemas y si existen diferencias entre una extremidad y la otra.
Fig. 10 Varices en ortostatismo
La palpación nos pondrá de manifiesto la tensión venosa aumentada en las varices, así como la existencia o no de dolor. A nivel de las venas perforantes apreciaremos el ojal que dejan éstas al atravesar la aponeurosis muscular.
Existen una serie de maniobras exploratorias (Schwartz, Tredelemburg, Bernstein y Pertes) que han quedado obsoletas tras la introducción del eco-doppler.
19.3.7 Exploraciones Complementarias
Especialmente útil es el eco-doppler. Con este sistema podemos explorar todos los trayectos venosos superficiales y profundos de las extremidades. Debe realizarse con el paciente tanto acostado como de pie y es una prueba no dolorosa, que no precisa ninguna preparación previa, que no usa contrastes y con una gran fiabilidad diagnóstica. La combinación de la ecografía con el efecto doppler nos permite ver las venas en todo su trayecto y comprobar no solo la insuficiencia valvular sino que podemos valorar en su interior si existen trombos, detectar anomalías del flujo venoso y mapear toda la anatomía y extensión de la enfermedad venosa. Estos estudios serán tanto más exactos según la calidad del equipo utilizado y la experiencia del explorador.
Fig. 11 Equipo eco-doppler
Otro tipo de pruebas como las flebografías (radiografías tras la inyección de contraste en las venas), AngioRNM, AngioTAC, flebografía isotópica,… son pruebas que pueden utilizarse para casos concretos como complemento a los estudios con eco-doppler.
Fig. 12 Flebografía
19.3.8 Tratamiento
Las varices son, en sus diferentes formas, una enfermedad degenerativa, progresiva y que generalmente no es grave pero si molesta y antiestética. En muchos casos el tratamiento es paliativo, en otros pueden curarse definitivamente.
Por tanto deben tratarse: las varices desarrolladas, las que han producido alteraciones en la piel o grasa subcutánea y aquellas en que queremos evitar futuras complicaciones (riesgo de tromboflebitis, úlceras o hemorragias). Por motivos puramente estéticos pueden tratarse las varices reticulares o las arañas vasculares.
Existen cuatro grupos de tratamientos que pueden o deben ser utilizados de forma conjunta:
1.- Medidas físico-higiénicas: consisten en la corrección de los factores predisponentes. Los pacientes con varices deben evitar la obesidad, corregir el estreñimiento, corregir las alteraciones ortopédicas y realizar ejercicios que favorezcan el retorno venoso mediante el desarrollo de la musculatura gemelar. Es fundamental la higiene cuidadosa y la hidratación de la piel de las piernas. En la mayoría de los casos es recomendable el uso de medias elásticas de compresión normal.
2ª.- Fármacos: existen numerosos tónicos venosos que actúan sobre la pared de la vena o mejorando la reabsorción del trasudado. Solo son útiles como medidas complementarias a las descritas previamente.
3ª.- Escleroterapia: consiste en la introducción en el interior de la vena de líquidos o espumas que producen una inflamación y obstrucción de la vena con la posterior desaparición de la red venosa. El tipo y concentración del producto esclerosante está en relación con el tamaño y localización de la vena. No todas las varices pueden ser tratadas con este método y existe un porcentaje de recidivas aunque su uso se ha extendido más desde la introducción de la microespuma. Se usa también como complemento a la cirugía.
Fig. 13 Esclerosis con polidocanol
Fig. 14 Preparando espuma para una esclerosis de la vena safena interna
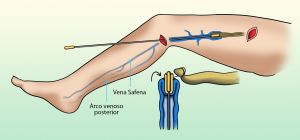
4º.- Cirugía: el método tradicional ha consistido en la extracción de las venas safena interna y/o externa mediante el arrancamiento con un “cable” asociado a la ligadura o cierre de sus uniones con las venas femoral o poplítea. Sus ramas colaterales se extraían mediante microincisiones según la técnica de Müller. Al cabo de 10 años hay un 25% de recidivas locales.
Fig. 15 Disección de cayado de vena safena interna
Fig. 16 Disección de la vena safena a nivel maleolar
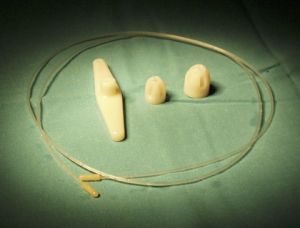
Fig. 17 Fleboextractor o stripper
Fig. 18 Mecanismo de extracción de vena safena interna
Fig. 19 Vena safena extraída
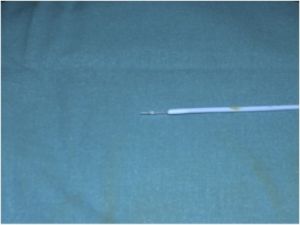
Recientemente se han introducido técnicas endovasculares menos invasivas como el endoláser o la radiofrecuencia. Son procedimientos quirúrgicos que evitan el “arrancamiento” de la vena safena sustituyéndolo por la eliminación de ldicha vena mediante un potente haz de luz (láser) u ondas de radio (radiofrecuencia) que “queman” la vena desde su luz. Se asocian a la técnica de Müller (microflebectomías) para eliminar simultáneamente las colaterales varicosas de las safenas. Tienen resultados similares a la cirugía convencional pero son menos agresivas y el post-operatorio es menos doloroso.
Fig. 20 Mecanismo actuación radiofrecuencia
Fig. 21 Punta de fibra de endoláser para varices
Fig. 22 Flebectomía de colaterales según técnica de Müller
Otra técnica en uso desde hace unos años es el método CHIVA o cirugía hemodinámica venosa. Los fundamentos teóricos de esta técnica son muy discutidos a nivel internacional y aunque algunos autores comunican buenos resultados se asocia a muchas reintervenciones posteriores. En casos seleccionados puede ser eficaz.
19.3.9 Complicaciones Secundarias a los Tratamientos
Ningún tratamiento médico o quirúrgico está exento de riesgos en ningún área de la Medicina.
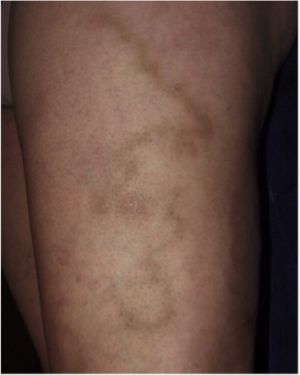
La escleroterapia puede asociarse a quemaduras químicas de la piel, tatuajes parduscos en el trayecto donde estuvo la variz, tromboflebitis de las venas profundas y embolismos pulmonares (especialmente en casos tratados con espuma). Son poco frecuentes pero pueden ser largos de resolver.
La cirugía tiene también una baja tasa de complicaciones pero están descritos hemorragias, hematomas organizados, infecciones de las heridas quirúrgicas, trombosis de las venas profundas, alteraciones sensitivas en el trayecto de los nervios safenos,… etc.
Fig. 23 Tatuaje post esclerosis
Fig. 24 Ulcera post esclerosis
19.3.10 Complicaciones de las Varices
Las cuatro complicaciones más frecuentes que pueden aparecer a lo largo de la evolución de unas varices no tratadas son:
- Varicorragia, o sangrado por rotura de una vena varicosa erosionando la piel. Como todo sangrado su aparición es muy llamativa pero no suele revestir mayor gravedad. Hay que tratarlas con elevación de la extremidad y un vendaje compresivo.
- Varicoflebitis, que es la formación de un coágulo en el interior de una variz. Es relativamente frecuente en las grandes varices y se presentan como un cordón duró, doloroso y eritematoso (rojizo). Si no se extiende el trombo a la zona próxima a la unión de la safena con la femoral o con la poplítea no supone gran peligro. Existen diferentes formas de tratamiento, desde la extracción quirúrgica del trombo hasta el uso de heparinas subcutáneas o antiinflamatorios según el criterio del médico en relación con la situación y gravedad del trombo.
Fig. 25 Varicoflebitis de una colateral de la vena safena interna
- Úlceras varicosas. Son dolorosas y de curación lenta. Se tratan mediante limpieza local, elevación de la extremidad y vendajes muy compresivos. Existen también numerosas pomadas, parches y otros productos que ayudan a la curación de la úlcera.
Fig. 26 Úlcera varicosa activa
- Dermatitis. Son inflamaciones de la piel, enrojecidas y que producen picor y desazón. Se tratan con pomadas corticoides, medias elásticas y eliminando la variz subyacente que la ha producido.
19.4 Bibliografía
1. Medicina Vascular. Complemento de Braunwald. Tratado de Cardiología. 2ª Edición. Mark A. Greager, Joshua A. Beckman. Edt Elservier Saunders. 2013
2. Rutherford´s Vascular Surgery. 8Th Edition. Rutherford. Jack L. Cronenwett MD, K. Wayne Jhonston. Elservier Saunders 2014.
3. Brand FN, Dannenberg AL, Abbott RD, Kannel WB. The epidemiology of varicose veins: the Framingham Study. Am J Prev Med 1988; 4:96.
4. Brittenden J, Cotton SC, Elders A, et al. A randomized trial comparing treatments for varicose veins. N Engl J Med 2014; 371:1218.
5. Rasmussen L, Lawaetz M, Bjoern L, et al. Randomized clinical trial comparing endovenous laser ablation and stripping of the great saphenous vein with clinical and duplex outcome after 5 years. J Vasc Surg 2013; 58:421.
6. O'Donnell TF Jr, Passman MA. Clinical practice guidelines of the Society for Vascular Surgery (SVS) and the American Venous Forum (AVF)--Management of venous leg ulcers. Introduction. J Vasc Surg 2014; 60:1S.
7. Labropoulos N, Tiongson J, Pryor L, et al. Definition of venous reflux in lower-extremity veins. J Vasc Surg 2003; 38:793.
8. Gloviczki P, Comerota AJ, Dalsing MC, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg 2011; 53:2S.
9. Management of Chronic Venous Disease. Clinical Practice of the European Society for Vascular Surgery.EurJVascEndovascSurg (2015)49,678e737
10. The care of patients with varicose veins and associated chronic venous disease: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. 2011, 53:1S-68S
11. Update in Venous Disease. 2011, 54:1S-76S
12. Sella D, Oldemburg A. Complication of inferior vena cava filters. Seminars in vascular Surgery. 2013, 26:23-28
13. Lohr J, Bush R. Venous disease in women: epidemiology, manifestations, and treatment. J Vasc Surg 57:37S-45S. 2013
14. Kaplan, R.M., Criqui, M.H., Denenberg, J.O., Bergan, J., and Fronek, A. Quality of life in patients with chronic venous disease: San Diego population study. J Vasc Surg. 2003; 37: 1047–1053
15. Smith, J.J., Guest, M.G., Greenhalgh, R.M., and Davies, A.H. Measuring the quality of life in patients with venous ulcers. J Vasc Surg. 2000; 31: 642–649
16. Korn, P., Patel, S.T., Heller, J.A., Deitch, J.S., Krishnasastry, K.V., Bush, H.L. et al. Why insurers should reimburse for compression stockings in patients with chronic venous stasis. J Vasc Surg. 2002; 35: 950–957
17. Coleridge-Smith, P., Labropoulos, N., Partsch, H., Myers, K., Nicolaides, A., Cavezzi, A. et al. Duplex ultrasound investigation of the veins in chronic venous disease of the lower limbs: UIP consensus document: part I(Basic principles) . Eur J Vasc Endovasc Surg. 2006; 31: 83–92
18. Hoggan, B.L., Cameron, A.L., and Maddern, G.J. Systematic review of endovenous laser therapy versus surgery for the treatment of saphenous varicose veins. Ann Vasc Surg. 2009; 23: 277–287
19. Mundy, L., Merlin, T.L., Fitridge, R.A., and Hiller, J.E. Systematic review of endovenous laser treatment for varicose veins. Br J Surg. 2005; 92: 1189–1194
20. Luebke, T., Gawenda, M., Heckenkamp, J., and Brunkwall, J. Meta-analysis of endovenous radiofrequency obliteration of the great saphenous vein in primary varicosis. J Endovasc Ther. 2008; 15: 213–223
21. Luebke, T. and Brunkwall, J. Systematic review and meta-analysis of endovenous radiofrequency obliteration, endovenous laser therapy, and foam sclerotherapy for primary varicosis. J Cadiovasc Surg. 2008; 49: 213–233
22. Jia, X., Mowatt, G., Burr, J.M., Cassar, K., Cook, J., and Fraser, C. Systematic review of foam sclerotherapy for varicose veins. Br J Surg. 2007; 94: 925–936
23. Leopardi, D., Hoggan, B.L., Fitridge, R.A., Woodruff, P.W., and Maddern, G.J. Systematic review of treatments for varicose veins. Ann Vasc Surg. 2009; 23: 264–276
24. Murad, M.H., Coto-Yglesias, F., Zumaeta-Garcia, M., Elamin, M.B., Duggirala, M.K., Erwin, P.J. et al. A systematic review and meta-analysis of the treatments of varicose veins. J Vasc Surg. 2011; 53: 51S–67S
25. Meissner, M.H., Gloviczki, P., Bergan, J., Kistner, R.L., Morrison, N., Pannier, F. et al. Primary chronic venous disorders. J Vasc Surg. 2007; 46: 54S–67S
26. Gloviczki, P. Do we need evidence-based medicine in the field of venous diseases?. Perspect Vasc Surg Endovasc Ther. 2004; 16: 129–133
27. O'Donnell, T.F. Jr and Lau, J. A systematic review of randomized controlled trials of wound dressings for chronic venous ulcer. J Vasc Surg. 2006; 44: 1118–1125
28. O'Donnell, T.F. Jr. The present status of surgery of the superficial venous system in the management of venous ulcer and the evidence for the role of perforator interruption. J Vasc Surg. 2008; 48: 1044–1052
29. Meissner, M.H. “I enjoyed your talk, but…”: evidence-based medicine and the scientific foundation of the American Venous Forum. J Vasc Surg. 2009; 49: 244–248
30. Partsch, H., Flour, M., and Smith, P.C. Indications for compression therapy in venous and lymphatic disease consensus based on experimental data and scientific evidence: under the auspices of the IUP. Int Angiol. 2008; 27: 193–219
31. Nicolaides, A.N., Allegra, C., Bergan, J., Bradbury, A., Cairols, M., Carpentier, P. et al. Management of chronic venous disorders of the lower limbs: guidelines according to scientific evidence. Int Angiol. 2008; 27: 1–59
32. Hirsh, J., Guyatt, G., Albers, G.W., Harrington, R., Schunemann, H.J., and American College of Chest Physicians. Antithrombotic and thrombolytic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008; 133: 110S–112S
33. Khilnani, N.M., Grassi, C.J., Kundu, S., D'Agostino, H.R., Khan, A.A., McGraw, J.K. et al. Multi-society consensus quality improvement guidelines for the treatment of lower-extremity superficial venous insufficiency with endovenous thermal ablation from the Society of Interventional Radiology, Cardiovascular Interventional Radiological Society of Europe, American College of Phlebology and Canadian Interventional Radiology Association. J Vasc Interv Radiol. 2010; 21: 14–31
34. Rabe, E., Pannier-Fischer, F., Gerlach, H., Breu, F.X., Guggenbichler, S., Zabel, M. et al. Guidelines for sclerotherapy of varicose veins (ICD 10: I83.0, I83.1, I83.2, and I83.9). Dermatol Surg. 2004; 30: 687–693
35. Robson, M.C., Cooper, D.M., Aslam, R., Gould, L.J., Harding, K.G., Margolis, D.J. et al. Guidelines for the treatment of venous ulcers. Wound Repair Regen. 2006; 14: 649–662
36. Agus, G.B., Allegra, C., Antignani, P.L., Arpaia, G., Bianchini, G., Bonadeo, P. et al. Guidelines for the diagnosis and therapy of the vein and lymphatic disorders. Int Angiol. 2005; 24: 107–168
37. Luebke, T. and Brunkwall, J. Meta-analysis of subfascial endoscopic perforator vein surgery (SEPS) for chronic venous insufficiency. Phlebology. 2009; 24: 8–16
38. Luebke, T. and Brunkwall, J. Meta-analysis of transilluminated powered phlebectomy for superficial varicosities. J Cadiovasc Surg. 2008; 49: 757–764
39. Palfreyman, S.J. and Michaels, J.A. A systematic review of compression hosiery for uncomplicated varicose veins. Phlebology. 2009; 24: 13–33
40. Scurr, J.R., Gilling-Smith, G.L., and Fisher, R.K. Systematic review of foam sclerotherapy for varicose veins (Br J Surg 2007; 94: 925-936). Br J Surg. 2007; 94: 1307–1308
41. Tenbrook, J.A. Jr, Iafrati, M.D., O'Donnell, T.F. Jr, Wolf, M.P., Hoffman, S.N., Pauker, S.G. et al. Systematic review of outcomes after surgical management of venous disease incorporating subfascial endoscopic perforator surgery. J Vasc Surg. 2004; 39: 583–589
42. Bamigboye, A.A. and Smyth, R. Interventions for varicose veins and leg oedema in pregnancy. Cochrane Database Syst Rev. 2007; (CD001066)
43. Tisi, P.V., Beverley, C., and Rees, A. Injection sclerotherapy for varicose veins. Cochrane Database Syst Rev. 2006; (CD001732)
44. O'Meara, S., Cullum, N.A., and Nelson, E.A. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2009; (CD000265)
45. Palfreyman, S.J., Nelson, E.A., Lochiel, R., and Michaels, J.A. Dressings for healing venous leg ulcers. Cochrane Database Syst Rev. 2006; (CD001103)
46. Meissner, M.H., Eklof, B., Smith, P.C., Dalsing, M.C., DePalma, R.G., Gloviczki, P. et al. Secondary chronic venous disorders. J Vasc Surg. 2007; 46: 68–83S
47. Meissner, M.H., Moneta, G., Burnand, K., Gloviczki, P., Lohr, J.M., Lurie, F. et al. The hemodynamics and diagnosis of venous disease. J Vasc Surg. 2007; 46: 4–24S
48. Henke, P., Writing Group I of the Pacific Vascular Symposium 6, Vandy, F., Comerota, A., Kahn, S.R., Lal, B.K. et al. Prevention and treatment of the postthrombotic syndrome. J Vasc Surg. 2010; 52: 21S–28S
49. Henke, P., Kistner, B., Wakefield, T.W., Eklof, B., and Lurie, F. Reducing venous stasis ulcers by fifty percent in 10 years: the next steps. J Vasc Surg. 2010; 52: 37S–38S
50. P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009
51. Guyatt, G., Gutterman, D., Baumann, M.H., Addrizzo-Harris, D., Hylek, E.M., Phillips, B. et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force. Chest. 2006; 129: 174–181
52. Caggiati, A., Bergan, J.J., Gloviczki, P., Eklof, B., Allegra, C., Partsch, H. et al. Nomenclature of the veins of the lower limb: extensions, refinements, and clinical application. J Vasc Surg. 2005; 41: 719–724
53. Mozes, G. and Gloviczki, P. New discoveries in anatomy and new terminology of leg veins: clinical implications. Vasc Endovasc Surg. 2004; 38: 367–374
54. Eklof, B., Perrin, M., Delis, K.T., Rutherford, R.B., Gloviczki, P. et al. Updated terminology of chronic venous disorders: the VEIN-TERM transatlantic interdisciplinary consensus document. J Vasc Surg. 2009; 49: 498–501
55. Caggiati, A., Bergan, J.J., Gloviczki, P., Jantet, G., Wendell-Smith, C.P., Partsch, H. et al. Nomenclature of the veins of the lower limbs: an international interdisciplinary consensus statement. J Vasc Surg. 2002; 36: 416–422
56. Kistner, R.L. and Eklof, B. Classification and etiology of chronic venous disease. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 37–46
57. Raju, S. and Neglén, P. Clinical practice(Chronic venous insufficiency and varicose veins) . N Engl J Med. 2009; 360: 2319–2327
58. Eberhardt, R.T. and Raffetto, J.D. Chronic venous insufficiency. Circulation. 2005; 111: 2398–2409
59. Rabe, E. and Pannier, F. Epidemiology of chronic venous disorders. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 105–110
60. Heit, J.A., Silverstein, M.D., Mohr, D.N., Petterson, T.M., Lohse, C.M., O'Fallon, W.M. et al. The epidemiology of venous thromboembolism in the community. Thromb Hemost. 2001; 86: 452–463
61. Carpentier, P.H., Maricq, H.R., Biro, C., Ponçot-Makinen, C.O., and Franco, A. Prevalence, risk factors, and clinical patterns of chronic venous disorders of lower limbs: a population-based study in France. J Vasc Surg. 2004; 40: 650–659
62. McLafferty, R.B., Passman, M.A., Caprini, J.A., Rooke, T.W., Markwell, S.A., Lohr, J.M. et al. Increasing awareness about venous disease: the American Venous Forum expands the national venous screening program. J Vasc Surg. 2008; 48: 394–399
63. Henke, P. The Pacific Vascular Symposium 6: the Venous Ulcer Summit in perspective. J Vasc Surg. 2010; 52: 1S–2S
64. Delis, K.T., Knaggs, A.L., and Khodabakhsh, P. Prevalence, anatomic patterns, valvular competence, and clinical significance of the Giacomini vein. J Vasc Surg. 2004; 40: 1174–1183
65. Gloviczki, P. and Mozes, G. Development and anatomy of the venous system. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 12–24
66. Langer, R.D., Ho, E., Denenberg, J.O., Fronek, A., Allison, M., Criqui, M.H. et al. Relationships between symptoms and venous disease: the San Diego population study. Arch Intern Med. 2005; 165: 1420–1424
67. Bradbury, A. and Ruckley, C.V. Clinical presentation and assessment of patients with venous disease. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 331–341
68. , P., van Rij, A.M., Christie, R.A., Hill, G.B., and Thomson, I.A. Non-saphenofemoral venous reflux in the groin in patients with varicose veins. Eur J Vasc Endovasc Surg. 2001; 21: 550–557
69. Gloviczki, P. and Driscoll, D.J. Klippel-Trenaunay syndrome: current management. Phlebology. 2007; 22: 291–298
70. Gloviczki, P., Duncan, A., Kalra, M., Oderich, G., Ricotta, J., Bower, T. et al. Vascular malformations: an update. Perspect Vasc Surg Endovasc Ther. 2009; 21: 133–148
71. Eklöf, B., Rutherford, R.B., Bergan, J.J., Carpentier, P.H., Gloviczki, P., Kistner, R.L. et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004; 40: 1248–1252
72. Vasquez, M.A., Rabe, E., McLafferty RB Shortell, C.K., Marston, W.A., Gillespie, D. et al. Revision of the venous clinical severity score: venous outcomes consensus statement: Special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. 2010; 52: 1387–1396
73. Cavezzi, A., Labropoulos, N., Partsch, H., Ricci, S., Caggiati, A., Myers, K. et al. Duplex ultrasound investigation of the veins in chronic venous disease of the lower limbs—UIP consensus document. Part II. Anatomy. Eur J Vasc Endovasc Surg. 2006; 31: 288–299
74. Labropoulos, N., Tiongson, J., Pryor, L., Tassiopoulos, A.K., Kang, S.S., Ashraf Mansour, M. et al. Definition of venous reflux in lower-extremity veins. J Vasc Surg. 2003; 38: 793–798
75. Labropoulos, N. Vascular diagnosis of venous thrombosis. in: M.A. Mansour, N. Labropoulos (Eds.) Vascular diagnosis. Elsevier Saunders, Philadelphia; 2005: 429–438
76. Park, U.J., Yun, W.S., Lee, K.B., Rho, Y.N., Kim, Y.W., Joh, J.H. et al. Analysis of the postoperative hemodynamic changes in varicose vein surgery using air plethysmography. J Vasc Surg. 2010; 51: 634–638
77. Lurie, F. and Rooke, T.W. Evaluation of venous function by indirect non-invasive testing (plethysmography). in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 156–159
78. Neglen, P. and Raju, S. Intravascular ultrasound scan evaluation of the obstructed vein. J Vasc Surg. 2002; 35: 694–700
79. Reed, N.R., Kalra, M., Bower, T.C., Vrtiska, T.J., Ricotta, J.J. 2nd, Gloviczki, P. et al. Left renal vein transposition for nutcracker syndrome. J Vasc Surg. 2009; 49: 386–393
80. Labropoulos, N., Manalo, D., Patel, N.P., Tiongson, J., Pryor, L., Giannoukas, A.D. et al. Uncommon leg ulcers in the lower extremity. J Vasc Surg. 2007; 45: 568–573
81. Rutherford, R.B., Moneta, G.L., Padberg, F.T. Jr, and Meissner, M.H. Outcome assessment in chronic venous disease. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 684–693
82. Pannier, F., Hoffmann, B., Stang, A., Jockel, K.-H., and Rabe, E. Prevalence and acceptance of therapy with medical compression stockings: results of the Bonn Vein Study. Phlebologie. 2007; 36: 245–249
83. Davies, A.H. and Rudarakanchana, N. Qualify of life and outcome assessment in patients with varicose veins. in: A.H. Davies, T.A. Lees, I.F. Lane (Eds.) Venous disease simplified. TFM Publishing Ltd, Shropshire, UK; 2006
84. Vasquez, M.A. and Munschauer, C.E. Venous Clinical Severity Score and quality-of-life assessment tools: application to vein practice. Phlebology. 2008; 23: 259–275
85. Lamping, D.L., Schroter, S., Kurz, X., Kahn, S.R., and Abenhaim, L. Evaluation of outcomes in chronic venous disorders of the leg: development of a scientifically rigorous, patient-reported measure of symptoms and quality of life. J Vasc Surg. 2003; 37: 410–419
86. Franks, P.J. and Moffatt, C.J. Health related quality of life in patients with venous ulceration: use of the Nottingham health profile. Qual Life Res. 2001; 10: 693–700
87. Wiebe, S., Guyatt, G., Weaver, B., Matijevic, S., and Sidwell, C. Comparative responsiveness of generic and specific quality-of-life instruments. J Clin Epidemiol. 2003; 56: 52–60
88. Kahn, S.R., M'Lan, C.E., Lamping, D.L., Kurz, X., Berard, A., Abenhaim, L.A. et al. Relationship between clinical classification of chronic venous disease and patient-reported quality of life: results from an international cohort study. J Vasc Surg. 2004; 39: 823–828
89. Launois, R., Mansilha, A., and Jantet, G. International psychometric validation of the Chronic Venous Disease quality of life Questionnaire (CIVIQ-20). Eur J Vasc Endovasc Surg. 2010; 40: 783–789
90. Ricci, M.A., Emmerich, J., Callas, P.W., Rosendaal, F.R., Stanley, A.C., Naud, S. et al. Evaluating chronic venous disease with a new venous severity scoring system. J Vasc Surg. 2003; 38: 909–915
91. Rutherford, R.B., Padberg, F.T. Jr, Comerota, A.J., Kistner, R.L., Meissner, M.H., Moneta, G.L. et al. Venous severity scoring: an adjunct to venous outcome assessment. J Vasc Surg. 2000; 31: 1307–1312
92. Meissner, M.H., Natiello, C., and Nicholls, S.C. Performance characteristics of the venous clinical severity score. J Vasc Surg. 2002; 36: 889–895
93. Mekako, A.I., Hatfield, J., Bryce, J., Lee, D., McCollum, P.T., and Chetter, I. A nonrandomised controlled trial of endovenous laser therapy and surgery in the treatment of varicose veins. Ann Vasc Surg. 2006; 20: 451–457
94. Gillet, J.L., Perrin, M.R., and Allaert, F.A. Clinical presentation and venous severity scoring of patients with extended deep axial venous reflux. J Vasc Surg. 2006; 44: 588–594
95. Kakkos, S.K., Rivera, M.A., Matsagas, M.I., Lazarides, M.K., Robless, P., Belcaro, G. et al. Validation of the new venous severity scoring system in varicose vein surgery. J Vasc Surg. 2003; 38: 224–228
96. Vasquez, M.A., Wang, J., Mahathanaruk, M., Buczkowski, G., Sprehe, E., Dosluoglu, H.H. et al. The utility of the Venous Clinical Severity Score in 682 limbs treated by radiofrequency saphenous vein ablation. J Vasc Surg. 2007; 45: 1008–1014
97. Vasquez, M.A., Rabe, E., McLaffertyt, R.B., Shortell, C.K., Marston, W.A., Gillespie, D. et al. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. 2010; 52: 1387–1396
98. Kundu, S., Lurie, F., Millward, S.F., Padberg, F. Jr, Vedantham, S., Elias, S. et al. Recommended reporting standards for endovenous ablation for the treatment of venous insufficiency: joint statement of the American Venous Forum and the Society of Interventional Radiology. J Vasc Surg. 2007; 46: 582–589
99. Perrin, M. and Allaert, F.A. Intra- and inter-observer reproducibility of the Recurrent Varicose Veins after Surgery (REVAS) classification. Eur J Vasc Endovasc Surg. 2006; 32: 326–332
100. Pittaluga, P., Chastanet, S., Rea, B., and Barbe, R. Midterm results of the surgical treatment of varices by phlebectomy with conservation of a refluxing saphenous vein. J Vasc Surg. 2009; 50: 107–118
101. Ramelet, A.A., Boisseau, M.R., Allegra, C., Nicolaides, A., Jaeger, K., Carpentier, P. et al. Veno-active drugs in the management of chronic venous disease(An international consensus statement: current medical position, prospective views and final resolution) . Clin Hemorheol Microcirc. 2005; 33: 309–319
102. Pittler, M.H. and Ernst, E. Horse chestnut seed extract for chronic venous insufficiency. Cochrane Database Syst Rev. 2006; (CD003230)
103. Coleridge-Smith, P., Lok, C., and Ramelet, A.A. Venous leg ulcer: a meta-analysis of adjunctive therapy with micronized purified flavonoid fraction. Eur J Vasc Endovasc Surg. 2005; 30: 198–208
104. Coleridge-Smith, P.D. Drug treatment of varicose veins, venous edema, and ulcers. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 359–365
105. Martinez, M.J., Bonfill, X., Moreno, R.M., Vargas, E., and Capella, D. Phlebotonics for venous insufficiency. Cochrane Database Syst Rev. 2005; (CD003229)
106. Nelson, E.A., Prescott, R.J., Harper, D.R., Gibson, B., Brown, D., Ruckley, C.V. et al. A factorial, randomized trial of pentoxifylline or placebo, four-layer or single-layer compression, and knitted viscose or hydrocolloid dressings for venous ulcers. J Vasc Surg. 2007; 45: 134–141
107. Hirsh, J., Guyatt, G., Albers, G.W., Harrington, R., and Schunemann, H.J. Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2006; 133: 71–109S
108. Moneta, G.L. and Partsch, H. Compression therapy for venous ulceration. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 348–358
109. Partsch, B. and Partsch, H. Calf compression pressure required to achieve venous closure from supine to standing positions. J Vasc Surg. 2005; 42: 734–738
110. Amsler, F. and Blattler, W. Compression therapy for occupational leg symptoms and chronic venous disorders: a meta-analysis of randomised controlled trials. Eur J Vasc Endovasc Surg. 2008; 35: 366–372
111. Michaels, J.A., Brazier, J.E., Campbell, W.B., MacIntyre, J.B., Palfreyman, S.J., and Ratcliffe, J. Randomized clinical trial comparing surgery with conservative treatment for uncomplicated varicose veins. Br J Surg. 2006; 93: 175–181
112. Michaels, J.A., Campbell, W.B., Brazier, J.E., Macintyre, J.B., Palfreyman, S.J., Ratcliffe, J. et al. Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial). Health Technol Assess. 2006; 10: 1–196
113. Ibegbuna, V., Delis, K.T., Nicolaides, A.N., and Aina, O. Effect of elastic compression stockings on venous hemodynamics during walking. J Vasc Surg. 2003; 37: 420–425
114. Zajkowski, P.J., Proctor, M.C., Wakefield, T.W., Bloom, J., Blessing, B., Greenfield, L.J. et al. Compression stockings and venous function. Arch Surg. 2002; 137: 1064–1068
115. Amsler, F., Willenberg, T., and Blättler, W. In search of optimal compression therapy for venous leg ulcers: a meta-analysis of studies comparing diverse [corrected] bandages with specifically designed stockings. J Vasc Surg. 2009; 50: 668–674
116. Partsch, H., Flour, M., and Smith, P.C. Indications for compression therapy in venous and lymphatic disease consensus based on experimental data and scientific evidence(Under the auspices of the IUP) . Int Angiol. 2008; 27: 193–219
117. Coleridge-Smith, P.D. Leg ulcer treatment. J Vasc Surg. 2009; 49: 804–808
118. Milic, D.J., Zivic, S.S., Bogdanovic, D.C., Perisic, Z.D., Milosevic, Z.D., Jankovic, R.J. et al. A randomized trial of the Tubulcus multilayer bandaging system in the treatment of extensive venous ulcers. J Vasc Surg. 2007; 46: 750–755
119. Barwell, J.R., Davies, C.E., Deacon, J., Harvey, K., Minor, J., Sassano, A. et al. Comparison of surgery and compression with compression alone in chronic venous ulceration (ESCHAR study): randomised controlled trial. Lancet. 2004; 363: 1854–1859
120. Gohel, M.S., Barwell, J.R., Taylor, M., Chant, T., Foy, C., Earnshaw, J.J. et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): randomised controlled trial. BMJ. 2007; 335: 83
121. Gardiner, R. and Negus, D. Compression hosiery: compression measurements and fitting. in: D. Negus, P.D. Coleridge-Smith, J.J. Bergan (Eds.) Leg ulcers: diagnosis and management. 3rd ed. Hodder Arnold, London; 2005: 227–232
122. Geerts, W.H., Bergqvist, D., Pineo, G.F., Heit, J.A., Samama, C.M., Lassen, M.R. et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133: 381–453S
123. Palfreyman, S., Nelson, E.A., and Michaels, J.A. Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ. 2007; 335: 244
124. Bergan, J.J. Varicose veins: hooks, clamps, and suction: application of new techniques to enhance varicose vein surgery. Semin Vasc Surg. 2002; 15: 21–26
125. Scavee, V., Lesceu, O., Theys, S., Jamart, J., Louagie, Y., Schoevaerdts, J.C. et al. Hook phlebectomy versus transilluminated powered phlebectomy for varicose vein surgery: early results. Eur J Vasc Endovasc Surg. 2003; 25: 473–475
126. Aremu, M.A., Mahendran, B., Butcher, W., Khan, Z., Colgan, M.P., Moore, D.J. et al. Prospective randomized controlled trial: conventional versus powered phlebectomy. J Vasc Surg. 2004; 39: 88–94
127. Chetter, I.C., Mylankal, K.J., Hughes, H., and Fitridge, R. Randomized clinical trial comparing multiple stab incision phlebectomy and transilluminated powered phlebectomy for varicose veins. Br J Surg. 2006; 93: 169–174
128. Rasmussen, L.H., Bjoern, L., Lawaetz, M., Lawaetz, B., Blemings, A., Eklof, B. et al. Randomised clinical trial comparing endovenous laser ablation with stripping of the great saphenous vein: clinical outcome and recurrence after 2 years. Eur J Vasc Endovasc Surg. 2010; 39: 630–635
129. Perkins, J.M. Standard varicose vein surgery. Phlebology. 2009; 24: 34–41
130. Menyhei, G., Gyevnar, Z., Arato, E., Kelemen, O., and Kollar, L. Conventional stripping versus cryostripping: a prospective randomised trial to compare improvement in quality of life and complications. Eur J Vasc Endovasc Surg. 2008; 35: 218–223
131. Kabnick, L.S. Phlebectomy. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 429–438
132. Lawrence, P.F. and Vardanian, A.J. Light-assisted stab phlebectomy: report of a technique for removal of lower extremity varicose veins. J Vasc Surg. 2007; 46: 1052–1054
133. Passman, M. Transilluminated powered phlebectomy in the treatment of varicose veins. Vascular. 2007; 15: 262–268
134. N., Elias, S.M., Keagy, B., Kolvenbach, R., Leahy, A.L., Marston, W. et al. Powered phlebectomy (trivex) in treatment of varicose veins. Ann Vasc Surg. 2002; 16: 488–494
135. Criado, E., Lujan, S., Izquierdo, L., Puras, E., Gutierrez, M., and Fontcuberta, J. Conservative hemodynamic surgery for varicose veins. Semin Vasc Surg. 2002; 15: 27–33
136. Zamboni, P., Cisno, C., Marchetti, F., Mazza, P., Fogato, L., Carandina, S. et al. Minimally invasive surgical management of primary venous ulcers vs. compression treatment: a randomized clinical trial. Eur J Vasc Endovasc Surg. 2003; 25: 313–318
137. Maeso, J., Juan, J., Escribano, J., Allegue, N.M., Di Matteo, A., Conzales, E. et al. Comparison of clinical outcome of stripping and CHIVA for treatment of varicose veins in the lower extremities. Ann Vasc Surg. 2001; 15: 661–665
138. Mowatt-Larssen, E. and Shortell, C. CHIVA. Semin Vasc Surg. 2010; 23: 118–122
139. Carandina, S., Mari, C., De Palma, M., Marcellino, M.G., Cisno, C., Legnaro, A. et al. Varicose vein stripping vs haemodynamic correction (CHIVA): a long term randomised trial. Eur J Vasc Endovasc Surg. 2008; 35: 230–237
140. Parés, J.O., Juan, J., Tellez, R., Mata, A., Moreno, C., Quer, F.X. et al. Varicose vein surgery: stripping versus the CHIVA method: a randomized controlled trial. Ann Surg. 2010; 251: 624–631
141. MacKenzie, R.K., Allan, P.L., Ruckley, C.V., and Bradbury, A.W. The effect of long saphenous vein stripping on deep venous reflux. Eur J Vasc Endovasc Surg. 2004; 28: 104–107
142. Sam, R.C., MacKenzie, R.K., Paisley, A.M., Ruckley, C.V., and Bradbury, A.W. The effect of superficial venous surgery on generic health-related quality of life. Eur J Vasc Endovasc Surg. 2004; 28: 253–256
143. Lurie, F., Creton, D., Eklof B Kabnick, L.S., Kistner, R.L., Pichot, O. et al. Prospective randomized study of endovenous radiofrequency obliteration (closure procedure) versus ligation and stripping in a selected patient population (EVOLVeS Study). J Vasc Surg. 2003; 38: 207–214
144. Frings, N., Nelle, A., Tran, P., Fischer, R., and Krug, W. Reduction of neoreflux after correctly performed ligation of the saphenofemoral junction: a randomized trial. Eur J Vasc Endovasc Surg. 2004; 28: 246–252
145. Winterborn, R.J., Foy, C., Heather, B.P., and Earnshaw, J.J. Randomised trial of flush saphenofemoral ligation for primary great saphenous varicose veins. Eur J Vasc Endovasc Surg. 2008; 36: 477–484
146. van Rij, A.M., Jones, G.T., Hill, B.G., Amer, M., Thomson, I.A., Pettigrew, R.A. et al. Mechanical inhibition of angiogenesis at the saphenofemoral junction in the surgical treatment of varicose veins: early results of a blinded randomized controlled trial. Circulation. 2008; 118: 66–74
147. Winterborn, R.J. and Earnshaw, J.J. Randomised trial of polytetrafluoroethylene patch insertion for recurrent great saphenous varicose veins. Eur J Vasc Endovasc Surg. 2007; 34: 367–373
148. Hayden, A. and Holdsworth, J. Complications following re-exploration of the groin for recurrent varicose veins. Ann R Coll Surg Engl. 2001; 83: 272–273
149. Hirsemann, S., Sohr, D., Gastmeier, K., and Gastmeier, P. Risk factors for surgical site infections in a free-standing outpatient setting. Am J Infect Control. 2005; 33: 6–10
150. Biswas, S., Clark, A., and Shields, D.A. Randomised clinical trial of the duration of compression therapy after varicose vein surgery. Eur J Vasc Endovasc Surg. 2007; 33: 631–637
151. Mekako, A.I., Chetter, I.C., Coughlin, P.A., Hatfield, J., and McCollum, P.T. Randomized clinical trial of co-amoxiclav versus no antibiotic prophylaxis in varicose vein surgery. Br J Surg. 2010; 97: 29–36
152. Atkin, G.K., Round, T., Vattipally, V.R., and Das, S.K. Common peroneal nerve injury as a complication of short saphenous vein surgery. Phlebology. 2007; 22: 3–7
153. Rudstrom, H., Bjorck, M., and Bergqvist, D. Iatrogenic vascular injuries in varicose vein surgery: a systematic review. World J Surg. 2007; 31: 228–233
154. van Rij, A.M., Chai, J., Hill, G.B., and Christie, R.A. Incidence of deep vein thrombosis after varicose vein surgery. Br J Surg. 2004; 91: 1582–1585
155. Scavee, V. Transilluminated powered phlebectomy: not enough advantages?(Review of the literature) . Eur J Vasc Endovasc Surg. 2006; 31: 316–319
156. Arumugasamy, M., McGreal, G., O'Connor, A., Kelly, C., Bouchier-Hayes, D., Leahy, A. et al. The technique of transilluminated powered phlebectomy: a novel, minimally invasive system for varicose vein surgery. Eur J Vasc Endovasc Surg. 2002; 23: 180–182
157. Shamiyeh, A., Schrenk, P., Huber, E., Danis, J., and Wayand, W.U. Transilluminated powered phlebectomy: advantages and disadvantages of a new technique. Dermatol Surg. 2003; 29: 616–619
158. Passman, M.A., Dattilo, J.B., Guzman, R.J., and Naslund, T.C. Combined endovenous ablation and transilluminated powered phlebectomy: is less invasive better?. Vasc Endovasc Surg. 2007; 41: 41–47
159. Franz, R.W. and Knapp, E.D. Transilluminated powered phlebectomy surgery for varicose veins: a review of 339 consecutive patients. Ann Vasc Surg. 2009; 23: 303–309
160. Blomgren, L., Johansson, G., Dahlberg-Akerman, A., Norén, A., Brundin, C., Nordström, E., and Bergqvist, D. Recurrent varicose veins: incidence, risk factors and groin anatomy. Eur J Vasc Endovasc Surg. 2004; 27: 269–274
161. Disselhoff, B.C., der Kinderen, D.J., Kelder, J.C., and Moll, F.L. Randomized clinical trial comparing endovenous laser with cryostripping for great saphenous varicose veins. Br J Surg. 2008; 95: 1232–1238
162. Perrin, M.R., Guex, J.J., Ruckley, C.V., dePalma, R.G., Royle, J.P., Eklof, B. et al. Recurrent varices after surgery (REVAS), a consensus document. Cardiovasc Surg. 2000; 8: 233–245
163. Fischer, R., Chandler, J.G., De Maeseneer, M.G., Frings, N., Lefebvre-Vilarbedo, M., Earnshaw, J.J. et al. The unresolved problem of recurrent saphenofemoral reflux. J Am Coll Surg. 2002; 195: 80–94
164. Allegra, C., Antignani, P.L., and Carlizza, A. Recurrent varicose veins following surgical treatment: our experience with five years follow-up. Eur J Vasc Endovasc Surg. 2007; 33: 751–756
165. Perrin, M.R., Labropoulos, N., and Leon, L.R. Jr. Presentation of the patient with recurrent varices after surgery (REVAS). J Vasc Surg. 2006; 43: 327–334
166. Fischer, R., Linde, N., Duff, C., Jeanneret, C., Chandler, J.G., Seeber, P. et al. Late recurrent saphenofemoral junction reflux after ligation and stripping of the greater saphenous vein. J Vasc Surg. 2001; 34: 236–240
167. Campbell, W.B., Vijay Kumar, A., Collin, T.W., Allington, K.L., and Michaels, J.A. Randomised and economic analysis of conservative and therapeutic interventions for varicose veins study(The outcome of varicose vein surgery at 10 years: clinical findings, symptoms and patient satisfaction) . Ann R Coll Surg Engl. 2003; 85: 52–57
168. Geier, B., Stücker, M., Hummel, T., Burger, P., Frings, N., Hartmann, M. et al. Residual stumps associated with inguinal varicose vein recurrences: a multicenter study. Eur J Vasc Endovasc Surg. 2008; 36: 207–210
169. Geier, B., Mumme, A., Hummel, T., Marpe, B., Stücker, M., Asciutto, G. et al. Validity of duplex-ultrasound in identifying the cause of groin recurrence after varicose vein surgery. J Vasc Surg. 2009; 49: 968–972
170. Asciutto, G., Asciutto, K.C., Mumme, A., and Geier, B. Pelvic venous incompetence: reflux patterns and treatment results. Eur J Vasc Endovasc Surg. 2009; 38: 381–386
171. Müller, M.A., Mayer, D., Seifert, B., Marincek, B., and Willmann, J.K. Recurrent lower-limb varicose veins: effect of direct contrast-enhanced three-dimensional MR venographic findings on diagnostic thinking and therapeutic decisions. Radiology. 2008; 247: 887–895
172. Creton, D. and Uhl, J.F. Foam sclerotherapy combined with surgical treatment for recurrent varicose veins: short term results. Eur J Vasc Endovasc Surg. 2007; 33: 619–624
173. Pittaluga, P., Chastanet, S., Locret, T., and Rousset, O. Retrospective evaluation of the need of a redo surgery at the groin for the surgical treatment of varicose vein. J Vasc Surg. 2010; 51: 1442–1450
174. van Groenendael, L., van der Vliet, J.A., Flinkenflögel l, L., Roovers, E.A., van Sterkenburg, S.M., Reijnen, M.M. et al. Treatment of recurrent varicose veins of the great saphenous vein by conventional surgery and endovenous laser ablation. J Vasc Surg. 2009; 50: 1106–1113
175. van Groenendael, L., Flinkenflogel, L., van der Vliet, J.A., Roovers, E.A., van Sterkenburg, S.M., and Reijnen, M.M. Conventional surgery and endovenous laser ablation of recurrent varicose veins of the small saphenous vein: a retrospective clinical comparison and assessment of patient satisfaction. Phlebology. 2010; 25: 151–157
176. O'Hare, J.L., Parkin, D., Vandenbroeck, C.P., and Earnshaw, J.J. Mid term results of ultrasound guided foam sclerotherapy for complicated and uncomplicated varicose veins. Eur J Vasc Endovasc Surg. 2008; 36: 109–113
177. Kabnick, L.S. Varicose veins: endovenous treatment. in: J.L. Cronenwett, K.W. Johnston (Eds.) Rutherford's vascular surgery. 7th ed. Saunders, Philadelphia; 2010: 871–888
178. van den Bos, R.R., Milleret, R., Neumann, M., and Nijsten, T. Proof-of-principle study of steam ablation as novel thermal therapy for saphenous varicose veins. J Vasc Surg. 2011; 53: 181–186
179. De Felice, E. Shedding light: laser physics and mechanism of action. Phlebology. 2010; 25: 11–28
180. Boné, C. Tratamiento endoluminal de las varices con laser de diodo: estudio preliminary. Rev Patol Vasc. 1999; 5: 35–46
181. Navarro, L., Min, R.J., and Boné, C. Endovenous laser: a new minimally invasive method of treatment for varicose veins: preliminary observations using an 810 nm diode laser. Dermatol Surg. 2001; 27: 117–122
182. Min, R.J., Zimmet, S.E., Isaacs, M.N., and Forrestal, M.D. Endovenous laser treatment of the incompetent greater saphenous vein. J Vasc Interv Radiol. 2001; 12: 1167–1171
183. Proebstle, T.M., Lehr, H.A., Kargl, A., Espinola-Klein, C., Rother, W., Bethge, S. et al. Endovenous treatment of the greater saphenous vein with a 940-nm diode laser: thrombotic occlusion after endoluminal thermal damage by laser-generated steam bubbles. J Vasc Surg. 2002; 35: 729–736
184. Proebstle, T.M., Moehler, T., Gül, D., and Herdemann, S. Endovenous treatment of the great saphenous vein using a 1,320 nm Nd:YAG laser causes fewer side effects than using a 940 nm diode laser. Dermatol Surg. 2005; 31: 1678–1683
185. Proebstle, T.M., Moehler, T., and Herdemann, S. Reduced recanalization rates of the great saphenous vein after endovenous laser treatment with increased energy dosing: definition of a threshold for the endovenous fluence equivalent. J Vasc Surg. 2006; 44: 834–839
186. Kalra, M. and Gloviczki, P. Fifteen years ago laser was supposed to open arteries, now it is supposed to close veins: what is the reality behind the tool?. Perspect Vasc Surg Endovasc Ther. 2006; 18: 3–8
187. Kabnick, L.S. Outcome of different endovenous laser wavelengths for great saphenous vein ablation. J Vasc Surg. 2006; 43: 88–93
188. Mozes, G., Kalra, M., Carmo, M., Swenson, L., and Gloviczki, P. Extension of saphenous thrombus into the femoral vein: a potential complication of new endovenous ablation techniques. J Vasc Surg. 2005; 41: 130–135
189. Puggioni, A., Kalra, M., and Gloviczki, P. Superficial vein surgery and SEPS for chronic venous insufficiency. Semin Vasc Surg. 2005; 18: 41–48
190. Puggioni, A., Kalra, M., Carmo, M., Mozes, G., and Gloviczki, P. Endovenous laser therapy and radiofrequency ablation of the great saphenous vein: analysis of early efficacy and complications. J Vasc Surg. 2005; 42: 488–493
191. Van den Bussche, D., Moreels, N., De Letter, J., and Lanckneus, M. Endovenous laser treatment for primary varicose veins. Acta Chir Belg. 2006; 106: 32–35
192. van den Bos, R., Arends, L., Kockaert, M., Neumann, M., and Nijsten, T. Endovenous therapies of lower extremity varicosities: a meta-analysis. J Vasc Surg. 2009; 49: 230–239
193. Stirling, M. and Shortell, C.K. Endovascular treatment of varicose veins. Semin Vasc Surg. 2006; 19: 109–115
194. Christenson, J.T., Gueddi, S., Gemayel, G., and Bounameaux, H. Prospective randomized trial comparing endovenous laser ablation and surgery for treatment of primary great saphenous varicose veins with a 2-year follow-up. J Vasc Surg. 2010; 52: 1234–1241
195. Chandler, J.G., Pichot, G., Sessa, C.S., Schuller-Petrović, S., Kabnick, L.S., and Bergan, J.J. Treatment of primary venous insufficiency by endovenous saphenous-vein obliteration. Vascul Surg. 2000; 34: 201–213
196. Chandler, J.G., Pichot, O., Sessa, C., Schuller-Petrović, S., Osse, F.J., Bergan, J.J. et al. Defining the role of extended saphenofemoral junction ligation: a prospective comparative study. J Vasc Surg. 2000; 32: 941–953
197. Pichot, O., Sessa, C., Chandler, J.G., Nuta, M., and Perrin, M. Role of duplex imaging in endovenous obliteration for primary venous insufficiency. J Endovasc Ther. 2000; 7: 451–459
198. Merchant, R.F., Pichot, O., and Closure Study Group. Long-term outcomes of endovenous radiofrequency obliteration of saphenous reflux as a treatment for superficial venous insufficiency. J Vasc Surg. 2005; 42: 502–509
199. Morrison, N. Saphenous ablation: what are the choices, laser or RF energy. Semin Vasc Surg. 2005; 18: 15–18
200. Lurie, F., Creton, D., Eklof, B., Kabnick, L.S., Kistner, R.L., Pichot, O. et al. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur J Vasc Endovasc Surg. 2005; 29: 67–73
201. Merchant, R.F., DePalma, R.G., and Kabnick, L.S. Endovascular obliteration of saphenous reflux: a multicenter study. J Vasc Surg. 2002; 35: 1190–1196
202. Hingorani, A.P., Ascher, E., Markevich, N., Schutzer, R.W., Kallakuri, S., Hou, A. et al. Deep venous thrombosis after radiofrequency ablation of greater saphenous vein: a word of caution. J Vasc Surg. 2004; 40: 500–504
203. Puggioni, A., Marks, N., Hingorani, A., Shiferson, A., Alhalbouni, S., Ascher, E. et al. The safety of
204. Proebstle, T.M., Vago, B., Alm, J., Göckeritz, O., Lebard, C., Pichot, O. et al. Treatment of the incompetent great saphenous vein by endovenous radiofrequency powered segmental thermal ablation: first clinical experience. J Vasc Surg. 2008; 47: 151–156
205. Gohel, M.S. and Davies, A.H. Radiofrequency ablation for uncomplicated varicose veins. Phlebology. 2009; 24: 42–49
206. Lawrence, P.F., Chandra, A., Wu, M., Rigberg, D., DeRubertis, B., Gelabert, H. et al. Classification of proximal endovenous closure levels and treatment algorithm. J Vasc Surg. 2010; 52: 388–393
207. Kabnick, L.S. Complications of endovenous therapies: statistics and treatment. Vascular. 2006; 14: S31–S32
208. Myers, K.A. and Jolley, D. Outcome of endovenous laser therapy for saphenous reflux and varicose veins: medium-term results assessed by ultrasound surveillance. Eur J Vasc Endovasc Surg. 2009; 37: 239–245
209. Rasmussen, L.H., Bjoern, L., Lawaetz, M., Blemings, A., Lawaetz, B., Eklof, B. et al. Randomized trial comparing endovenous laser ablation of the great saphenous vein with high ligation and stripping in patients with varicose veins: short-term results. J Vasc Surg. 2007; 46: 308–315
210. Min, R.J., Khilnani, N., and Zimmet, S.E. Endovenous laser treatment of saphenous vein reflux: long-term results. J Vasc Interv Radiol. 2003; 14: 991–996
211. Huisman, L.C., Bruins, R.M., van den Berg, M., and Hissink, R.J. Endovenous laser ablation of the small saphenous vein: prospective analysis of 150 patients, a cohort study. Eur J Vasc Endovasc Surg. 2009; 38: 199–202
212. Knipp, B.S., Blackburn, S.A., Bloom, J.R., Fellows, E., Laforge, W., Pfeifer, J.R. et al. Endovenous laser ablation: venous outcomes and thrombotic complications are independent of the presence of deep venous insufficiency. J Vasc Surg. 2008; 48: 1538–1545
213. Pannier, F., Rabe, E., and Maurins, U. First results with a new 1470-nm diode laser for endovenous ablation of incompetent saphenous veins. Phlebology. 2009; 24: 26–30
214. Doganci, S. and Demirkilic, U. Comparison of 980 nm laser and bare-tip fibre with 1470 nm laser and radial fibre in the treatment of great saphenous vein varicosities: a prospective randomised clinical trial. Eur J Vasc Endovasc Surg. 2010; 40: 254–259
215. Darwood, R.J., Theivacumar, N., Dellagrammaticas, D., Mavor, A.I., and Gough, M.J. Randomized clinical trial comparing endovenous laser ablation with surgery for the treatment of primary great saphenous varicose veins. Br J Surg. 2008; 95: 294–301
216. de Medeiros, C.A. and Luccas, G.C. Comparison of endovenous treatment with an 810 nm laser versus conventional stripping of the great saphenous vein in patients with primary varicose veins. Dermatol Surg. 2005; 31: 1685–1694 (discussion: 1694)
217. Vuylsteke, M., Van den Bussche, D., Audenaert, E.A., and Lissens, P. Endovenous laser obliteration for the treatment of primary varicose veins. Phlebology. 2006; 21: 80–87
218. Kalteis, M., Berger, I., Messie-Werndl, S., Pistrich, R., Schimetta, W., Pölz, W. et al. High ligation combined with stripping and endovenous laser ablation of the great saphenous vein: early results of a randomized controlled study. J Vasc Surg. 2008; 47: 822–829 (discussion: 829)
219. Pronk, P., Gauw, S.A., Mooij MC Gaastra, M.T., Lawson, J.A., van Goethem, A.R. et al. Randomised controlled trial comparing sapheno-femoral ligation and stripping of the great saphenous vein with endovenous laser ablation (980 nm) using local tumescent anaesthesia: one year results. Eur J Vasc Endovasc Surg. 2010; 40: 649–656
220. Thakur, B., Shalhoub, J., Hill, A.M., Gohel, M.S., and Davies, A.H. Heterogeneity of reporting standards in randomised clinical trials of endovenous interventions for varicose veins. Eur J Vasc Endovasc Surg. 2010; 40: 528–533
221. Nicolini, P. Treatment of primary varicose veins by endovenous obliteration with the VNUS closure system: results of a prospective multicentre study. Eur J Vasc Endovasc Surg. 2005; 29: 433–439
222. Rautio, T., Ohinmaa, A., Perälä, J., Ohtonen, P., Heikkinen, T., Wiik, H. et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: a randomized controlled trial with comparison of the costs. J Vasc Surg. 2002; 35: 958–965
223. Pichot, O., Kabnick, L.S., Creton, D., Merchant, R.F., Schuller-Petroviae, S., Chandler, J.G. et al. Duplex ultrasound scan findings two years after great saphenous vein radiofrequency endovenous obliteration. J Vasc Surg. 2004; 39: 189–195
224. Hinchliffe, R.J., Ubhi, J., Beech, A., Ellison, J., and Braithwaite, B.D. A prospective randomised controlled trial of VNUS closure versus surgery for the treatment of recurrent long saphenous varicose veins. Eur J Vasc Endovasc Surg. 2006; 31: 212–218
225. Perala, J., Rautio, T., Biancari, F., Ohtonen, P., Wiik, H., Heikkinen, T. et al. Radiofrequency endovenous obliteration versus stripping of the long saphenous vein in the management of primary varicose veins: 3-year outcome of a randomized study. Ann Vasc Surg. 2005; 19: 669–672
226. Gale, S.S., Lee, J.N., Walsh, M.E., Wojnarowski, D.L., and Comerota, A.J. A randomized, controlled trial of endovenous thermal ablation using the 810-nm wavelength laser and the ClosurePLUS radiofrequency ablation methods for superficial venous insufficiency of the great saphenous vein. J Vasc Surg. 2010; 52: 645–650
227. Shepherd, A.C., Gohel, M.S., Brown, L.C., Metcalfe, M.J., Hamish, M., and Davies, A.H. Randomized clinical trial of VNUS ClosureFAST radiofrequency ablation versus laser for varicose veins. Br J Surg. 2010; 97: 810–818
228. Almeida, J.I., Kaufman, J., Göckeritz, O., Chopra, P., Evans, M.T., Hoheim, D.F. et al. Radiofrequency endovenous ClosureFAST versus laser ablation for the treatment of great saphenous reflux: a multicenter, single-blinded, randomized study (RECOVERY study). J Vasc Interv Radiol. 2009; 20: 752–759
229. Marston, W.A., Owens, L.V., Davies, S., Mendes, R.R., Farber, M.A., and Keagy, B.A. Endovenous saphenous ablation corrects the hemodynamic abnormality in patients with CEAP clinical class 3–6 CVI due to superficial reflux. Vasc Endovasc Surg. 2006; 40: 125–130
230. Guex, J.J., Allaert, F.A., Gillet, J.L., and Chleir, F. Immediate and midterm complications of sclerotherapy: report of a prospective multicenter registry of 12,173 sclerotherapy sessions. Dermatol Surg. 2005; 31: 123–128
231. Cornu-Thenard, A., de Cottreau, H., and Weiss, R.A. Sclerotherapy: continuous wave Doppler-guided injections. Dermatol Surg. 1995; 21: 867–870
232. Cabrera Garido, J.R., Cabrera Garcia Olmedo, J.R., and Olmedo, D.G. Nuevo metododel de esclerosis en las varices tronculares. Patol Vasculares. 1995; 4: 55–73
233. Cabrera, J., Redondo, P., Becerra, A., Garrido, C., Cabrera, J. Jr, García-Olmedo, M.A. et al. Ultrasound-guided injection of polidocanol microfoam in the management of venous leg ulcers. Arch Dermatol. 2004; 140: 667–673
234. Cabrera, J., Cabrera, J. Jr, Garcia-Olmedo, M.A., and Redondo, P. Treatment of venous malformations with sclerosant in microfoam form. Arch Dermatol. 2003; 139: 1409–1416
235. Cavezzi, A. and Tessari, L. Foam sclerotherapy techniques: different gases and methods of preparation, catheter versus direct injection. Phlebology. 2009; 24: 247–251
236. Frullini, A. and Cavezzi, A. Sclerosing foam in the treatment of varicose veins and telangiectases: history and analysis of safety and complications. Dermatol Surg. 2002; 28: 11–15
237. Coleridge-Smith, P. Foam and liquid sclerotherapy for varicose veins. Phlebology. 2009; 24: 62–72
238. Smith, P.C. Chronic venous disease treated by ultrasound guided foam sclerotherapy. Eur J Vasc Endovasc Surg. 2006; 32: 577–583
239. Barrett, J.M., Allen, B., Ockelford, A., and Goldman, M.P. Microfoam ultrasound-guided sclerotherapy of varicose veins in 100 legs. Dermatol Surg. 2004; 30: 6–12
240. Breu, F.X., Guggenbichler, S., and Wollmann, J.C. 2nd. European Consensus Meeting on Foam sclerotherapy 2006,Tegernsee, Germany. Vasa. 2008; 37: 1–29
241. Breu, F.X. and Guggenbichler, S. European Consensus Meeting on Foam Sclerotherapy, April 4-6, 2003, Tegernsee, Germany. Dermatol Surg. 2004; 30: 709–717
242. Bountouroglou, D.G., Azzam, M., Kakkos, S.K., Pathmarajah, M., Young, P., Geroulakos, G. et al. Ultrasound-guided foam sclerotherapy combined with sapheno-femoral ligation compared to surgical treatment of varicose veins: early results of a randomised controlled trial. Eur J Vasc Endovasc Surg. 2006; 31: 93–100
243. Kakkos, S.K., Bountouroglou, D.G., Azzam, M., Kalodiki, E., Daskalopoulos, M., Geroulakos, G. et al. Effectiveness and safety of ultrasound-guided foam sclerotherapy for recurrent varicose veins: immediate results. J Endovasc Ther. 2006; 13: 357–364
244. Tessari, L., Cavezzi, A., and Frullini, A. Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg. 2001; 27: 58–60
245. Bergan, J. Sclerotherapy: a truly minimally invasive technique. Perspect Vasc Surg Endovasc Ther. 2008; 20: 70–72
246. Bergan, J. and Cheng, V. Foam sclerotherapy for the treatment of varicose veins. Vascular. 2007; 15: 269–272
247. O'Hare, J.L., Stephens, J., Parkin, D., and Earnshaw, J.J. Randomized clinical trial of different bandage regimens after foam sclerotherapy for varicose veins. Br J Surg. 2010; 97: 650–656
248. Guex, J.J. Complications and side-effects of foam sclerotherapy. Phlebology. 2009; 24: 270–274
249. Bergan, J.J., Weiss, R.A., and Goldman, M.P. Extensive tissue necrosis following high-concentration sclerotherapy for varicose veins. Dermatol Surg. 2000; 26: 535–541
250. Ceulen, R.P., Sommer, A., and Vernooy, K. Microembolism during foam sclerotherapy of varicose veins. N Engl J Med. 2008; 358: 1525–1526
251. Munavalli, G.S. and Weiss, R.A. Complications of sclerotherapy. Semin Cutan Med Surg. 2007; 26: 22–28
252. Bush, R.G., Derrick, M., and Manjoney, D. Major neurological events following foam sclerotherapy. Phlebology. 2008; 23: 189–192
253. Picard, C., Deltombe, B., Duru, C., Godefroy, O., and Bugnicourt, J.M. Foam sclerotherapy: a possible cause of ischaemic stroke?. J Neurol Neurosurg, Psychiatry. 2010; 81: 582–583
254. Forlee, M.V., Grouden, M., Moore, D.J., and Shanik, G. Stroke after varicose vein foam injection sclerotherapy. J Vasc Surg. 2006; 43: 162–164
255. Morrison, N., Cavezzi, A., Bergan, J., and Partsch, H. Regarding Stroke after varicose vein foam injection sclerotherapy. J Vasc Surg. 2006; 44: 224–225
256. Wright, D., Gobin, J.P., Bradbury, A.W., Coleridge-Smith, P., Spoelstra, H., Berridge, D. et al. Varisolve polidocanol microfoam compared with surgery or sclerotherapy in the management of varicose veins in the presence of trunk vein incompetence: European randomized controlled trial. Phlebology. 2006; 21: 180–190
257. Regan, J.D., Gibson, K.D., Rush, J.E., Shortell, C.K., Hirsch, S.A., and Wright, D.D. Clinical significance of cerebrovascular gas emboli during polidocanol endovenous ultra-low nitrogen microfoam ablation and correlation with magnetic resonance imaging in patients with right-to-left shunt. J Vasc Surg. 2011; 53: 131–170
258. Morrison, N., Neuhardt, D.L., Rogers, C.R., McEown, J., Morrison, T., Johnson, E. et al. Comparisons of side effects using air and carbon dioxide foam for endovenous chemical ablation. J Vasc Surg. 2008; 47: 830–836
259. Kern, P., Ramelet, A.A., Wütschert, R., and Hayoz, D. Compression after sclerotherapy for telangiectasias and reticular leg veins: a randomized controlled study. J Vasc Surg. 2007; 45: 1212–1216
260. Goldman, M.P. Treatment of varicose and telangiectatic leg veins: double-blind prospective comparative trial between aethoxyskerol and sotradecol. Dermatol Surg. 2002; 28: 52–55
261. Rabe, E., Otto, J., Schliephake, D., and Pannier, F. Efficacy and safety of great saphenous vein sclerotherapy using standardised polidocanol foam (ESAF): a randomised controlled multicentre clinical trial. Eur J Vasc Endovasc Surg. 2008; 35: 238–245
262. Yamaki, T., Nozaki, M., and Iwasaka, S. Comparative study of duplex-guided foam sclerotherapy and duplex-guided liquid sclerotherapy for the treatment of superficial venous insufficiency. Dermatol Surg. 2004; 30: 718–722
263. Cabrera, J., Cabrera, J. Jr, and Garcia-Olmedo, M.A. Sclerosants in microfoam: a new approach in angiology. Int Angiol. 2001; 20: 322–329
264. Darvall, K.A., Sam, R.C., Bate, G.R., Silverman, S.H., Adam, D.J., Bradbury, A.W. et al. Changes in health-related quality of life after ultrasound-guided foam sclerotherapy for great and small saphenous varicose veins. J Vasc Surg. 2010; 51: 913–920
265. Rigby, K.A., Palfreyman, S.J., Beverley, C., and Michaels, J.A. Surgery versus sclerotherapy for the treatment of varicose veins. Cochrane Database Syst Rev. 2004; (CD004980)
266. Perrin, M. Endovenous radiofrequency ablation of saphenous vein reflux. The VNUS Closure procedure with Closurefast. An updated review. Int Angiol. 2010; 29: 303–307
267. Enzler, M.A. and van den Bos, R.R. A new gold standard for varicose vein treatment?. Eur J Vasc Endovasc Surg. 2010; 39: 97–98
268. Masuda, E.M., Kessler, D.M., Lurie, F., Puggioni, A., Kistner, R.L., Eklof, B. et al. The effect of ultrasound-guided sclerotherapy of incompetent perforator veins on venous clinical severity and disability scores. J Vasc Surg. 2006; 43: 551–556
269. Whiteley, M.S., Holdstock, J.M., Price, B.A., Smith, J.J., and Gallagher, T.M. Radiofrequency ablations of the refluxing great saphenous vein system, Giacomini veins, incompetent perforating veins using VNUS closure and TRLOP technique. Phlebology. 2003; 18: 52
270. Peden, E. and Lumsden, A. Radiofrequency ablation of incompetent perforator veins. Perspect Vasc Surg Endovasc Ther. 2007; 19: 73–77
271. Hingorani, A.P., Ascher, E., Marks, N., Shiferson, A., Patel, N., Gopal, K. et al. Predictive factors of success following radio-frequency stylet (RFS) ablation of incompetent perforating veins (IPV). J Vasc Surg. 2009; 50: 844–848
272. Marks, N., Hingorani, A., and Ascher, E. New office-based vascular interventions. Perspect Vasc Surg Endovasc Ther. 2008; 20: 340–345
273. O'Donnell, T.F. The role of perforators in chronic venous insufficiency. Phlebology. 2010; 25: 3–10
274. Elias, S. Percutaneous ablation of perforating veins. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 536–544
275. Proebstle, T.M. and Herdemann, S. Early results and feasibility of incompetent perforator vein ablation by endovenous laser treatment. Dermatol Surg. 2007; 33: 162–168
276. Kianifard, B., Holdstock, J., Allen, C., Smith, C., Price, B., and Whiteley, M.S. Randomized clinical trial of the effect of adding subfascial endoscopic perforator surgery to standard great saphenous vein stripping. Br J Surg. 2007; 94: 1075–1080
277. van Neer, P., Kessels, F.G., Estourgie, R.J., de Haan, E.F., Neumann, M.A., Veraart, J.C. et al. Persistent reflux below the knee after stripping of the great saphenous vein. J Vasc Surg. 2009; 50: 831–834
278. Nelzen, O. Prospective study of safety, patient satisfaction and leg ulcer healing following saphenous and subfascial endoscopic perforator surgery. Br J Surg. 2000; 87: 86–91
279. Iafrati, M.D., Pare, G.J., O'Donnell, T.F., and Estes, J. Is the nihilistic approach to surgical reduction of superficial and perforator vein incompetence for venous ulcer justified?. J Vasc Surg. 2002; 36: 1167–1174
280. Kalra, M., Gloviczki, P., Noel, A.A., Rooke, T.W., Lewis, B.D., Jenkins, G.D. et al. Subfascial endoscopic perforator vein surgery in patients with post-thrombotic venous insufficiency: is it justified?. Vasc Endovasc Surg. 2002; 36: 41–50
281. Kalra, M. and Gloviczki, P. Subfascial endoscopic perforator vein surgery: who benefits?. Semin Vasc Surg. 2002; 15: 39–49
282. Bianchi, C., Ballard, J.L., Abou-Zamzam, A.M., and Teruya, T.H. Subfascial endoscopic perforator vein surgery combined with saphenous vein ablation: results and critical analysis. J Vasc Surg. 2003; 38: 67–71
283. Tawes, R.L., Barron, M.L., Coello, A.A., Joyce, D.H., and Kolvenbach, R. Optimal therapy for advanced chronic venous insufficiency. J Vasc Surg. 2003; 37: 545–551
284. Rhodes, J.M., Kalra, M., and Gloviczki, P. The management of incompetent perforating veins with open and endoscopic surgery. in: P. Gloviczki (Ed.) Handbook of venous disorders: guidelines of the American Venous Forum. 3rd ed. Hodder Arnold, London; 2009: 523–535
285. Coakley, F.V., Varghese, S.L., and Hricak, H. CT and MRI of pelvic varices in women. J Comput Assist Tomogr. 1999; 23: 429–434
286. Chung, M.H. and Huh, C.Y. Comparison of treatments for pelvic congestion syndrome. Tohoku J Exp Med. 2003; 201: 131–138